Non-operative Treatment and PRP for Tommy John Injuries
Summary of non-operative treatment
- Rest from throwing
- Ice, NSAIDS
- PRP injections
- Strengthening program focusing on forearm, shoulder, leg, hip, core
- Progressive throwing program with symptoms resolve and exam normal
- Changing position to decrease stress on elbow (move from pitcher to first base)
- Pitching mechanics optimization
What are your goals?
Non-operative treatment requires careful consideration of the patient’s athletic expectations in addition to consideration of the degree of UCL injury. Seasonal and career timing are also important to consider. Athletes with low demands who are less serious about continuing with baseball may choose to play first base rather than a high-demand position such as pitching as they undergo non-operative treatment. Players with aspirations of playing at the collegiate or professional level, may opt for more immediate surgical reconstruction.
Initial Non-op Treatment
Initial non-operative treatment for UCL injury consists of rest, ice, anti-inflammatory medication and, in some cases, use of an elbow brace. This is aimed at reducing pain and inflammation and allowing initial healing. We highly discourage cortisone injections into the area of the UCL. Platelet-rich plasma (PRP) is a treatment that can accelerate healing and improve the quality of healing.
Platelet-Rich Plasma
PRP injections are used to treat ligament and tendon injuries and can enhance healing of UCL tears. PRP therapy is part of a relatively new field of medicine known as orthobiologics that includes the use of stem cells and emphasizes the latest technologies along with the body’s natural ability to heal itself.
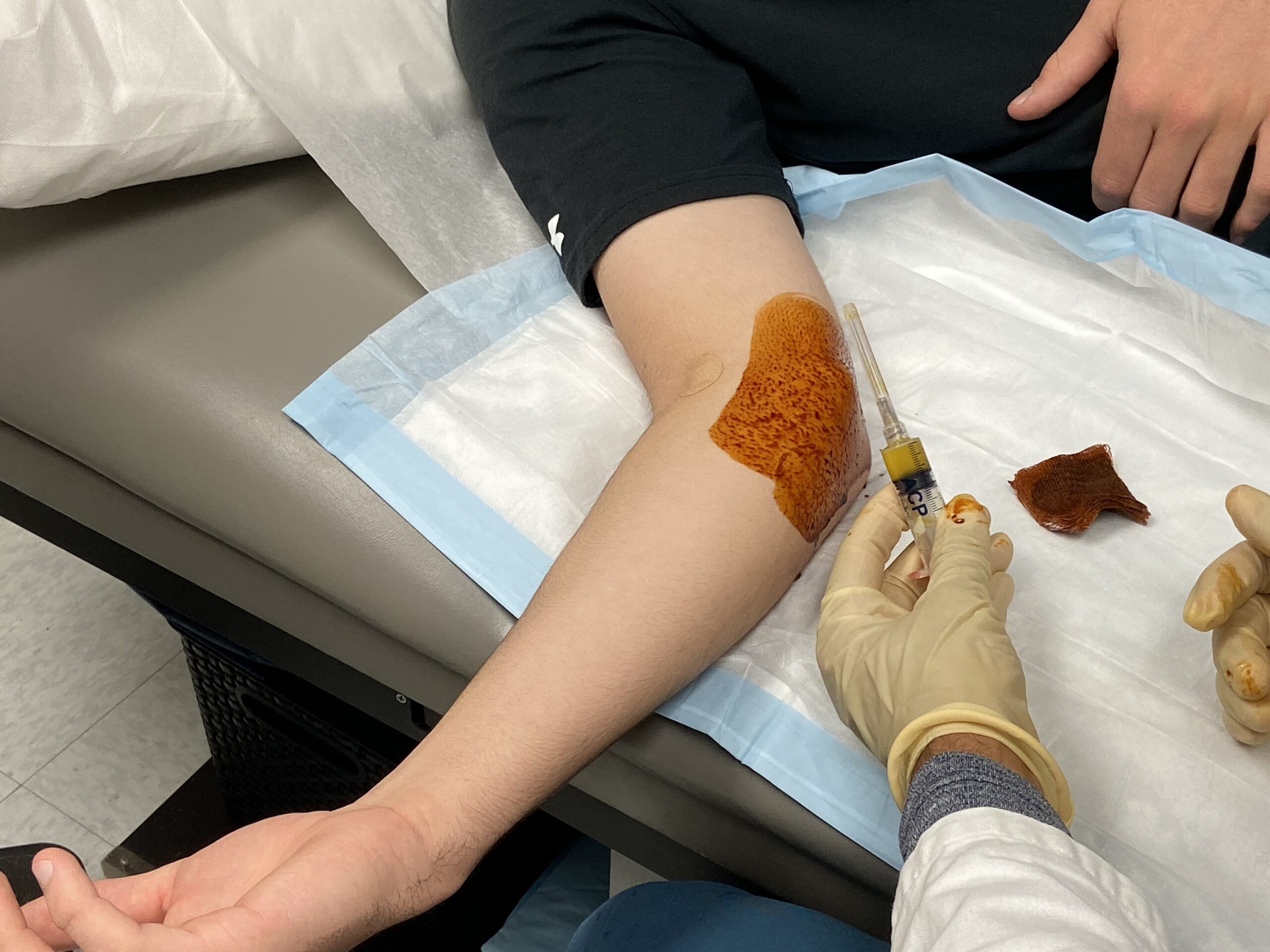
Our blood is made of red blood cells, white blood cells, plasma, and platelets. Platelet-rich plasma is the name given to blood plasma with a high concentration of platelets that contains huge doses of bioactive proteins, such as growth factors, that are critical in the repair and regeneration of tissues. To extract these platelets, a small amount of blood is drawn from the patient and immediately undergoes centrifugation, a process in which mixtures are separated using centripetal force. This process separates out red blood cells, which carry oxygen, and the platelets and the plasma. The platelets with the plasma have all of the healing agents. Once we’ve done the separation, we extract the PRP that can then be injected back into the patient’s injured area. It is their own platelet-rich plasma — it isn’t taken from another person or derived in a laboratory.
Growth factors can dramatically enhance tissue recovery and the special proteins also initiate new blood vessel formation, bone regeneration and healing, connective tissue repair, and wound healing. There is little chance for rejection because the components used for treatment are extracted from a person’s own body. This makes the procedure entirely safe. The PRP injection also carries less chance for infection than an incision, with a considerably shorter recovery time than after surgery.
I began using PRP therapy as an option for professional athletes. Once we established that this approach was beneficial for the professional, I began offering it to young athletes. We have an even greater motivation to use a healing agent for younger patients. The younger a patient is, the less we want to operate, which is potentially career ending if it doesn’t work, or could possibly change the normal anatomy. We try to preserve a patient’s own anatomy and tissues and avoid surgery as much as possible.
I have researched the effects of injury in younger children and adolescents as compared to adults. Preliminary data shows that a sports injury in an adolescent has much greater impact on his or her emotional status and perception of quality of life. That makes sense because adults work and have other responsibilities. With students, their focus and energy are on school, socializing and, often, athletics. If you take away their ability to be involved in athletics, it affects their school and social environment. Young athletes have so much future and potential, and if we don’t provide the maximum benefit to them, they have a long life to feel the repercussions.
As Director of Biomechanics Research at the Center for Orthopaedic Research, I continue to explore the uses and benefits of PRP. We know that the platelet-rich plasma is working, but what we aren’t sure about yet is what the exact dosing should be. Is one injection enough? Are two injections better? Are three injections too many? So I’m involved in determining what the exact dose should be. Major League Baseball funded an ongoing study to determine the effects of repeated dosing and optimal timing between doses.
I participated in a clinical outcomes study with several colleagues to evaluate the effect of PRP injections on partial ulnar collateral ligament (UCL) tears in high-level throwing athletes. We reviewed the results of 44 baseball players (six professional, 14 college, 24 high school) treated with PRP injections whose mean age was 17.3 years. Of the 44 patients, 15 (34%) had an excellent outcome, 17 had a good outcome, two had a fair outcome, and 10 had a poor outcome. After injection, four (67%) of the six professional players returned to professional play. There were no injection-related complications. Our use of PRP in the treatment of UCL insufficiency produced outcomes much better than earlier reported outcomes of conservative treatment of these injuries. PRP injections may be particularly beneficial in young athletes who have sustained acute damage to an isolated part of the ligament and in athletes unwilling or unable to undergo the extended rehabilitation required after surgical reconstruction of the ligament.
The period of non-operative treatment with or without PRP is typically six weeks of no throwing. During the period of no throwing, physical therapy is started and designed to strengthen elbow, shoulder, hip and core muscles. When the physical examination determines no tenderness over the UCL and negative stress testing, a throwing program is initiated. Throwing mechanics are optimized and flexibility and strength is maintained in the lower extremities, trunk, and core muscles. Non-operative treatment typically takes three to four months before players are fully active.
Patients who wish to continue baseball but fail non-operative treatments, and maintain symptoms and the ability to throw are indicated for Tommy John surgery. A long and lengthy recovery is demanding both physically and mentally. Athletes need to be committed to achieving a favorable result.
See Dr. Ahmad perform a PRP injection to stimulate UCL healing
Physical Therapy
Physical therapy is used to correct muscle weakness or imbalances in the arm and also the entire kinetic chain. We use therapists who are highly skilled with taking care of baseball players and for athletes of all competitive levels, we coordinate care with their team athletic training staff. Non-operative therapy is similar to therapy that follows Tommy John Surgery
Throwing Programs
Throwing programs are individualized to the needs of players depending on the degree of injury, seasonal timing. Throwing programs are initiated with players are symptoms free and have normal physical exam. In addition, plyo ball throwing takes place before actual baseball throwing.
In 2009 a Yankee outfielder made a routine hard throw and felt a pop in his elbow. He was immediately examined and his UCL was tender. An MRI scan revealed his UCL was partially torn. This player wanted an alternative to surgery which is associated with a long recovery period. He was recommended to undergo PRP injections to the UCL injury with ultrasound guidance. He was able to rehab, and return to professional pitching while avoiding surgery.
Conservative treatment is often the first step in the management of ulnar collateral ligament (UCL) injuries, though it should be applied in the appropriate patient context. Specific features of the clinical history, injury mechanism, physical exam and imaging help Dr. Ahmad and the patient to pursue conservative treatment. Treatment is aimed at reducing elbow pain and inflammation prior to initiating active rehabilitation. The outcomes of non-operative management of UCL injury are often satisfactory with appropriate patient and injury.
MRI can predict the outcome of non-operative treatment. Research has shown that low-grade partial tears and tears-in-continuity did well with non-surgical rehabilitation in a cohort of 39 baseball players. Seasonal timing is an important consideration when deciding to move forward with conservative versus surgical management.
What about PRP?
Recent studies have favored biologic augmentation, specifically the use of platelet-rich-plasma (PRP). PRP stands for platelet-rich plasma, and contains high concentrations of platelets and growth factors that have been implicated in accelerating the healing process. PRP is obtained from a patient by drawing a small amount of blood (approximately 10-15 cc) and placing it in a centrifuge for the PRP to be separated from the other components of the blood. PRP is an alternative to surgery that uses ultrasound to precisely localize the injection to the exact area of injury.
How many injections should I have?
Dr. Ahmad recommends 3 PRP injections, each separated by one week.
Can physical therapy help?
Physical therapy can assist with kinetic chain strengthening including the core, lower extremities and flexor mass. Weakness of the core musculature has been shown to increase muscle compensations and increase load elsewhere, including spinal loading, shoulder, and elbow, which may predispose an athlete for injury.
When do I return to throwing?
Dr. Ahmad reexamines the patient at six weeks from the first injection. If the patient’s examination is improved, the patient can undergo a functional throwers assessment. A functional throwers assessment is administered by a physical therapist and evaluates the patient’s readiness to return to sport. Functional assessment includes evaluation of shoulder and elbow strength and endurance testing.
Upon completing of a throwers assessment, the athlete begins a return to throwing program which takes 6 weeks to complete. Additionally, pitchers must do an additional mound program before returning to a game situation. Pitchers may benefit from return to play as a position player to decrease the load on the UCL.
What does the research show?
A retrospective study of baseball players with isolated symptomatic partial UCL tears treated with platelet-rich-plasma yielded favorable outcomes. Ahmad and colleagues reported of 44 athletes treated with PRP, 15 returned to play with excellent outcomes, and 17 returned to play with good outcomes. Similarly, a study of 34 baseball players with partial or complete UCL tears that were treated with PRP injection resulted in 26 athletes being able to return to pre-injury level of play within six months (Kato). They reported a range of return to play time between 10-18 weeks, and an average of 12.4 weeks.