Overview
Cartilage Restoration
Over time your joint’s cartilage or—natural “shock absorbers”—wear down and become vulnerable to tears and chipping. This is typically the cause of cartilage damage in adults over the age of 30. However, younger athletes are not clear from the risks of cartilage damage—one of the most common causes of damage is from acute sports injury or overuse. Without healthy cartilage, your joints simply cannot function smoothly or effectively.
Your Cartilage is: The smooth, white tissue that covers the ends of bones where they come together to form joints.
The Facts on Cartilage Restoration:
- The most common cause of cartilage damage is normal wear and tear over time.
- Cartilage does not heal well on its own, making it difficult to treat damage.
- Damaged cartilage can lead to arthritis.
Symptoms:
In many cases, patients who have joint injuries, such as meniscal or ligament tears, will also have cartilage damage. Damage to cartilage, meniscus, and ligaments are all best diagnosed with an MRI.
The following symptoms are commonly reported by patients seeking cartilage treatment:
- Knee pain–this may continue even when resting, and worsen when bearing weight
- Swelling of the knee
- Stiffness
- A clicking or grinding feeling
- Locking or instability of the knee joint
Evaluation by Team Ahmad
Dr. Ahmad and his team of health professionals will greet you and start your visit with a discussion of your symptoms and your sport, level of competition, or desired activity level. Next, the doctor will exam your knee, focusing on:
- Your knee’s range of motion
- Swelling
- Location of tenderness
Imaging Tests: MRI and X-ray
Because other knee problems cause similar symptoms, Dr. Ahmad may order imaging tests to help confirm the diagnosis. The most commonly used scan is an MRI, but x-rays may also be considered.
Treatment Options
You may be eligible for articular cartilage restoration—especially if you are a young adult with minimal cartilage damage history. Cartilage restoration is a surgical technique to create new cartilage to replace the damaged cartilage.
Older patients, or those with many lesions in one joint, are less likely to benefit from the procedure.
Surgical
Arthroscopic surgery: One of the most commonly performed surgical procedures, includes inserting a miniature camera into the knee through a small incision. This provides a clear view of the inside of the knee. Dr. Ahmad uses tiny surgical instruments through other small incisions to trim or repair your damaged cartilage.
There are other surgical procedures that are used to restore cartilage, and require greater access to the cartilage.
Depending upon your specific needs, Dr. Ahmad and his team will discuss your options and help determine what kind of procedure is right for you.
The most common procedures for cartilage restoration are:
- Microfracture
- Drilling
- Abrasion Chondroplasty
- Osteochondral Allograft Transplantation
Microfracture
Goal:
Microfracture surgery aims to stimulate the growth of new articular cartilage cells by creating a new blood supply to the damaged area.
Process:
A sharp tool called a microfracture pick is used to make multiple holes in the joint surface, beneath the cartilage and within the bone. These activate a natural healing response—the perforations allow bone marrow with stem cells access to the cartilage injury that will help new cartilage to form.
Microfracture surgery can be done arthroscopically and is a procedure best suited for younger patients with smaller areas of cartilage damage.
Drilling
Goal:
Drilling, like the microfracture procedure, aims to stimulate the natural production of healthy cartilage.
Process:
Holes are drilled, using a surgical drill or wire, through the injured area in the bone beneath your cartilage. A natural healing response is triggered by drilling into the bone.
Abrasion Arthroplasty
Goal:
Abrasion arthroplasty is similar to the drilling and microfracture treatment options in that it aims to stimulate the natural recovery of the cartilage.
Process:
Using high speed burrs, Abrasion arthroplasty removes the damaged cartilage and exposes the bone beneath to bone marrow.
Osteochondral Autograft
Goal:
Osteochondral autograft transplantation aims to successfully transfer, healthy cartilage (a graft) from one part of the joint to another.
Process:
- Healthy cartilage tissue is removed from a non-weight carrying bone, to the affected area in the knee.
- The graft is taken as a cylinder-shaped plug of cartilage and bone beneath the cartilage.
- Next, the graft of healthy cartilage is matched to the surface of the defective cartilage and forced into place. This results in a smooth cartilage surface in the joint.
Osteochondral Allograft Transplantation
Goal:
An allograft aims to use a healthy a tissue sample taken from a cadaver donor, and transplant it to the affected area of the knee.
Process:
The allograft is a large cylinder of cartilage and bone. Prior to being transplanted it is sterilized and intensely tested to avoid any possible disease. An allograft is typically used to treat a larger affected area than is an autograft.
The transplanted sample, can be customized in terms of shape and depth, so that it exactly fits the contour of the cartilage defect. Allografts are typically done through an open incision.
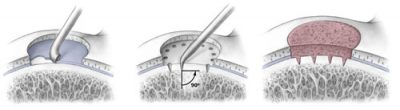
Steps of the microfracture technique. Left: Damaged cartilage is removed. Center: Microfracture pick instrument is used to make perforations in thebone. Right: Healing response brings bone marrow cells to the defect and forms new cartilage.
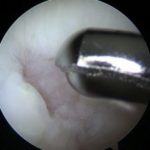
Abrasion arthroplasty can be done with an arthroscope.
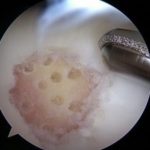
Articular cartilage damage in the knee (left). The cartilage damage after treatment with microfracture(right).
Rehabilitation and Recovery
Post-surgery rehabilitation typically includes:
- Placing no, or minimal, weight on the affected leg. You will need to use crutches to move around for the first few weeks of recovery.
- Physical therapy to help restore strength and mobility to the affected knee. This could include strength training and the use of a continuous motion machine, especially early in the recovery process.
- More aggressive strength training as healing progresses and normal functionality begins to return.
Please be aware that it may take several months of dedicated rehabilitation before you can safely return to sports or strenuous physical activity.
Dr. Ahmad’s Experience
Dr. Ahmad is nationally recognized expert in knee cartilage repair surgery and has designed and studied the optimal methods to repair knee cartilage defects. His undergraduate training in mechanical engineering has allowed him to research cartilage repair and understand what state of the art surgical techniques are best to offer his patients. Dr. Ahmad has performed nearly 1000 knee cartilage related surgeries in all types of patients from professional soccer players to those who training for their first marathon.
PUBLICATIONS and PRESENTATIONS
- Oungoulian SR, Durney KM, Jones BK, Ahmad CS, Hung CT, Ateshian GA: Wear and damage of articular cartilage with friction against orthopedic implant materials. J Biomech. 2015 Jul 16;48(10): 1957-64. Epub 2015 Apr 15.
- Oungoulian SR, Hehir KE, Zhu K, Willis CE, Marinescu AG, Merali N, Ahmad CS, Hung CT, Ateshian GA: Effect of glutaraldehyde fixation on the frictional response of immature bovine articular cartilage explants, J Biomech, 47(3):694-701, 2013
- Franzone J, Vitale M, Shubin Stein BE, Ahmad CS: Is there an Association between Chronicity of Patellar Instability and Patellofemoral Cartilage Lesions: An Arthroscopic Assessment of Chondral Injury, Journal of Knee Surgery, 25:411-416, 2012
- Caligaris M, Canal CE, Ahmad CS, Gardner TR, Ateshian GA: Investigation of the Frictional Response of Osteoarthritic Human Tibiofemoral Joints and the Potential Beneficial Tribological Effect of Healthy Synovial Fluid. Osteoarthritis and Cartilage, 17: 1327-1332, 2009
- Ahmad CS, Guiney WB, Drinkwater CR: Evaluation of Donor Site Intrinsic Healing Response in Osteochondral Grafting of the Knee. Arthroscopy, 18:95-98, 2002
- Ahmad CS, Cohen ZA, Levin e WN, Ateshian GA, Mow VC: Biomechanical and Topographic Considerations in Autologous Osteochondral Grafting in the Knee. American Journal of Sports Medicine, 29:201-206, 2001
- Cohen ZA, Ahmad CS, Roglic H, Levine WN, Henry JH, Ateshian GA, Mow VC: Biomechanical Considerations for Autologous Osteochondrol Grafting of the Femoral Articular Surface. American Society of Mechanical Engineers BED, 42: 129-130, 1999
- Kwak SD, Ateshian GA, Blankevoort L, Ahmad, CS, Gardner TR, Grelsamer RP, Henry JH, Mow VC: A General Mathematical Multibody Model for Diarthrodial Joints: Application and Validation Using the Patellofemoral Joint. American Society of Mechanical Engineers BED, 31: 239-240, 1996
- Xu LF, Ahmad CS, Strauch RJ, Wang VM, Wang LH, Rosenwasser MP, Pawluk RJ, Ateshian GA: New Method to Measure Congruence of the Thumb Carpometacarpal Joint: Maximum Contact Area Criterion. American Society of Mechanical Engineers BED, 31: 113-114, 1995
- Kwak SD, Blankevoort L, Ahmad CS, Gardner TR, Grelsamer RP, Henry JH, Ateshian GA, Mow VC: Anatomically Based 3-D Coordinate System for the Knee Joint. American Society of Mechanical Engineers BED, 31: 309-310, 1995
- Ateshian GA, Cohen ZA, Kwak SD, Wang VM, Ahmad CS, Kelkar R: Determination of In-Situ Contact Areas in Diarthrodial Joints by MRI. American Society of Mechanical Engineers BED, 31: 225-226, 1995
- Ahmad CS, Frenkel, Sally R, Casar RS, Alexander H: Mechanical Testing Technique for Articular Cartilage: A Study of Intrinsic Repair. American Society of Mechanical Engineers BED, 22: 379-382, 1992
Review Articles, Current Concept Articles and Surgical Techniques
Textbooks/ Guest Editorship
- Ahmad CS, Editor: Sports Medicine 2. Instructional Course Lectures Sports Medicine Specialty Volume 2: American Academy of Orthopaedic Surgeons, Illinois, 2011
- Ahmad CS, Shubin Stein BE Guest Editor: Patellar Instability. Operative Techniques in Sports Medicine. Elsevier, Illinois. Vol 18, pp 61-128, 2010
- Ahmad CS, Editor: American Academy of Orthopaedic Surgeons Monograph Series. Pediatric and Adolescent Sports Injuries. American Academy of Orthopaedic Surgeons. American Academy of Orthopaedic Surgeons, Rosemont. Series 43, pp 1-199, 2010
- Levine WN, Ahmad CS, Editors: Management of the Patellofemoral Joint. Operative Techniques in Orthopedic Surgery. Williams and Wilkins, Philadelphia. Vol 17, pp 203-264, 2007
- Ahmad CS, Cohen ZA, Levine WN, Ateshian GA, Mow VC: Biomechanical and Topographic Considerations for Osteochondral Grafting in the Knee. American Academy of Orthopaedic Surgeons Annual Meeting, Orlando FL, February 1999
- Ahmad CS, Kwak SD, Ateshian GA, Gardner TR, Blankevoort L, Warden WH, Grelsamer RP, Henry JH, Steadman JR, Mow VC: Adhesive Contracture of the Patellar Ligament: Effect on Patellar and Tibial Kinematics and Contact. Annual Meeting of the Orthopaedic Research Society, San Francisco CA, February 1997