Revision Tommy John Surgery
Second Time Tommy John Surgery
Increasing Tommy John Surgeries Equates to Increasing Second Tommy John Surgeries.
The number of Tommy John injuries in pitchers of all competitive levels has been increasing over the last 10 years. The success rates following Tommy John Surgery have been encouraging, with greater than 80% of patients commonly able to return to play at a high level. Unfortunately, as the number of Tommy John Surgeries continues to rise, the number of second time Tommy John Surgeries increase. Second Tommy John Surgery is commonly referred to as revision Tommy John Surgery. In MLB, there were more revision Tommy John Surgery in the 3 years from 2012 and 2014 than in the prior 12 years combined.
Reasons for the increase in revision Tommy John Surgery
- Number of increasing Tommy John Surgeries being performed, especially in younger patients
- Increased incentive to continue playing. Patients who, in the past, would have discontinued baseball with a failed Tommy John Surgery are now more incentivized to keep playing and undergo a revision.
Risk Factors for Needing a Second Tommy John Surgery
- Accelerating the recovery process. A shorter time from the Tommy John Surgery to return to play is associated with an increase risk of revision Tommy John Surgery.
- Increased workload. Another risk factor is an increase in pitching workload after Tommy John Surgery compared to before the injury.
- Unfortunately, younger age at the time of Tommy John Surgery (22.9 for those requiring revision Tommy John Surgery vs. 27.3 for those not requiring revision Tommy John Surgery) is another risk factor.
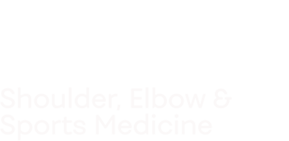
Pre-operative anteroposterior (AP) X-Ray on a patient with a failed ulnar collateral ligament reconstruction (Tommy John Surgery). The original humeral tunnel is marked by the green arrow. The original tunnel is very superficial and short, which does not allow adequate graft length to be placed into the humeral tunnel. Notice the calcification within the ligament (red arrow).
Dr. Ahmad explains Revision UCL Reconstruction
Patient Evaluation
History
Dr. Ahmad and his team will perform a thorough evaluation of a player when injury to his Tommy John Surgery is suspected.
Symptoms Similar to patients who sustain a tear of their native UCL but often less severe
- Medial elbow as well as loss of accuracy and velocity.
- The pain is often nagging, and continues to worsen over time.
- Alternatively, some patients complain of a single, distinct injury when they felt a “pop” in their elbow following a specific pitch, although this can happen, especially if the patient sustained a fracture through their one of their bone tunnels.
- Ahmad will obtain the operative report of the initial surgery if it was done by another surgeon. The graft choice, surgical technique (including surgical approach: muscle split vs. elevation), management of the ulnar nerve, and any concomitant elbow pathology is necessary information.
Imaging – X-rays, MRI, CT Scan, Ultrasound
- X-rays are carefully inspected for fracture through the prior tunnels, and to determine the position of the prior tunnels, and possible calcium deposits.
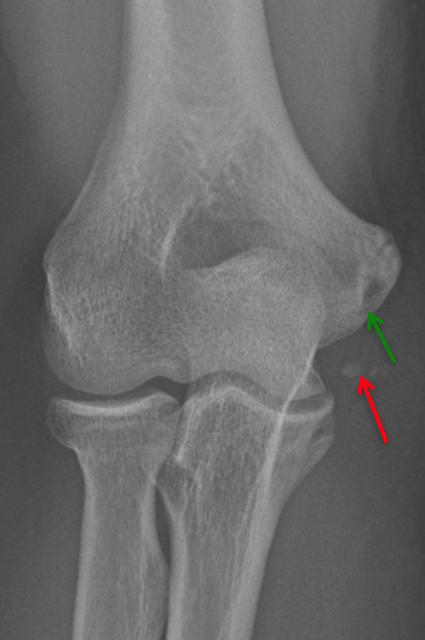
- MRI and MR arthrography (MRA) are used to evaluate the UCL graft as well as cartilage injuries, flexor pronator injuries, and bone stress injuries.
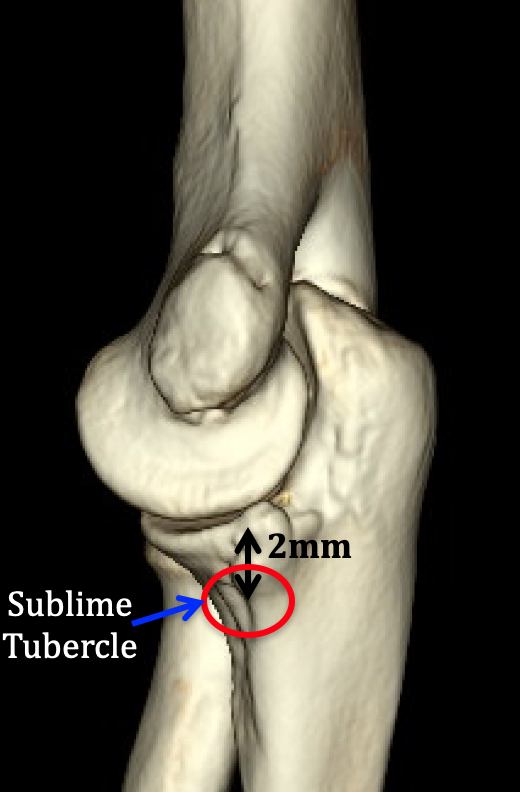
- CT scan is used to evaluate bone spurs and exact location of the prior ulnar and humeral tunnels as well as the bone quality of these tunnels. The tunnels can be assessed for widening, fracture, and malposition.
CT scan revealing superficial and posterior position of the humeral tunnel. The inferior aspect of the humeral tunnel should be at the 7 to 8 o’clock position. The tunnel in this case is at approximately the 5 o’clock position. If the tunnel is too posterior the graft will be tight in flexion and lose in extension, which led to failure in this case.
Physical Exam
Dr. Ahmad and his team will perform a physical exam of the patient with a presumed UCL re-tear similar to a patient who has not had prior surgery. There will be additional physical exam assessments.
- The location of the scar will be critically evaluated.
- The ulnar nerve location will be assessed.
- The prior graft harvest site is evaluated.
- Kinetic chain issues such as spine or core weakness, inflexibility, or muscle imbalance as well as improper throwing mechanics are assessed.
Tunnel Status
- The status of prior tunnels can have significant implications on the surgical technique used for the revision Tommy John Surgery.
- The ulnar tunnels should ideally be located 2 to 4 mm distal to the joint line and equidistant on both sides of the sublime tubercle. Sublime tubercle morphology can be altered by bone spurs. The medial ulnar ridge can serve as a guide to the proper location of the sublime tubercle.
- The inferior position of the humeral tunnel should start at least 5 mm anterior to the 6 o’clock position of the medial epicondyle.
- Malpositioned tunnels result in a non-isometric graft. For example, if the tunnels are placed too far posterior, which is a common error, this will result in a tight graft in flexion. As a result either elbow flexion will be limited or, if flexion is obtained, the graft subsequently becomes loose. A graft that is placed too superficial on the epicondyle will result in a small length of the epicondyle and will be less isometric.
Treatment
Non-Operative
- As with a tear of the native UCL, an injury to the reconstructed UCL can be managed initially in a non-operative manner.
- Non-operative treatment includes rest, rehabilitation, electrical stimulation, ultrasound, and other modalities used by therapists.
- Use of biologics such as platelet rich plasma (PRP) have shown positive results
Causes for Failure of Tommy John Surgery
- The causes of failure following primary Tommy John Surgery can be broken down into technical errors, patient factors, rehabilitation problems, or failure of the graft.
- Surgical technique errors include poor tunnel placement, improper tensioning of the graft, and poor graft fixation. If the medial epicondyle socket is not placed at the isometric point, it will cause the graft to load unevenly and can lead to increased stress seen by the graft and ultimate failure. Similarly, if the ulnar tunnel is not parallel to the joint surface, or is too proximal or too distal, it may lead to failure of the graft. If less than a 1cm bone bridge is left for the ulnar tunnel, or if the medial epicondyle socket is too far medial, these bone bridges can break and cause catastrophic failure. Depending on the surgical technique utilized, if the graft is not properly secured, it runs the risk of loosening over time.
- Patient factors can lead to failure of graft incorporation and ultimately failure of the primary Tommy John Surgery such as steroid use, smoking, and failure to comply with rehabilitation protocols. Likewise, if the patient does not participate in therapy, or if the therapy being given is not tailored to the specific patient, the pitcher may never optimize their throwing mechanics and can continue to improperly stress their UCL. Failure to achieve full shoulder and elbow range of motion (ROM) can put the pitcher at increased risk for a recurrent UCL tear.
- Finally, there is the chance that the UCL graft will degenerate and wear out over time. Studies have shown that pitchers who have their index Tommy John Surgery at earlier ages are more likely to require a revision Tommy John Surgery. This is likely because the number of pitches the reconstructed UCL sees in a younger patient is higher than in a pitcher at the end of their career.
Graft Choice for Revision Tommy John Surgery
- As in primary Tommy John Surgery, there are several graft choices available in the revision setting. If the index procedure was performed with an ipsilateral palmaris longus autograft, I prefer hamstring autograft.
Prior Ulnar Nerve Transposition
- If the patient had a previous ulnar nerve transposition, the nerve should be identified intraoperatively, isolated, protected, and re-transposed at the end of the procedure.
- Great care should be taken when isolating the nerve as this is often encased in scar tissue and can be easily injured.
Surgical Technique
- Revision Tommy John Surgery is much more complicated than first time Tommy John Surgery.
- If the patient had a fracture through their ulnar tunnel, or has significant widening on the ulnar or humeral tunnel, the standard docking technique may not be effective. Modifications to the technique may need to be made in order to properly secure the graft.
Dr. Ahmad’s Preferred Surgical Technique
Late Failure
If the patient had a well-functioning Tommy John Surgery (late failure) and physical exam and imaging studies indicate simple attenuation and failure of the graft without technical surgical error, Tommy John Surgery is carried out similar to a primary Tommy John Surgery. The previously existing tunnels are re-created and the graft choice is most often a gracilis tendon autograft.
Early failure
Sources of early failure include failure of graft incorporation, over accelerated rehabilitation, and surgical technical error. If the patient has a collagen disorder they may elect an allograft for their Tommy John Surgery. If the tunnels are malpositioned than the tunnels should be modified to a more accurate position. This usually involves either ignoring a previously used malpositioned tunnel if it is far from the normal position or, if it is close to its normal position, than the tunnel is created and a more precise location with partial overlap with the previous tunnel. A large gracilis tendon graft is commonly used.
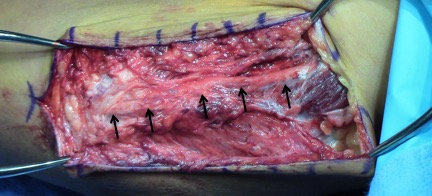
Set up and Exposure
- Patient set up is the same as for primary UCL reconstruction.
- The prior incision should be utilized. This may be extended proximally and distally.
- If the ulnar nerve has been previously transposed, a meticulous dissection of the ulnar nerve is carried out. Often the ulnar nerve is best identified proximally where there is less scar tissue.
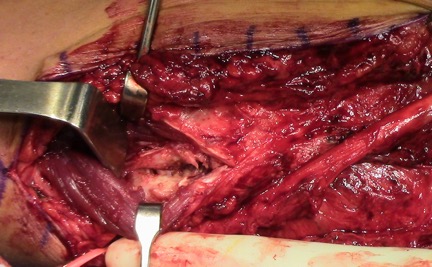
- A split in the flexor carpi ulnaris (FCU) fascia is created and the prior ligament graft is identified. The graft often has to be debulked.
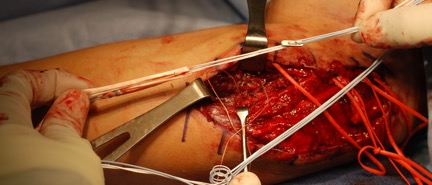
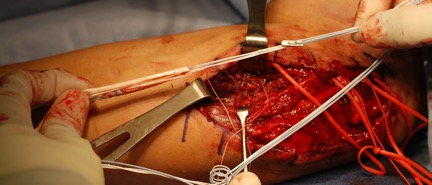
Image of a previous ulnar nerve transposition. The black arrows indicate the course of the ulnar nerve.
Intraoperative photo of graft failure. The black arrow indicates the failed graft.
Single ulnar tunnel socket creation. A pin is used to drill into the ulna at the level of the sublime tubercle (A). The pin is overdrilled using a reamer (B). A pin to shuttle the cortical button is then placed through the previously drilled socket (C).
Graft prepared with cortical button for ulnar fixation.
Ulnar tunnels
- The medial ulnar ridge on the ulna is used to help identify the proper location of the sublime tubercle. Small curettes are used to identify the prior tunnel on the ulna, both anterior and posterior to the sublime tubercle. If the tunnel position and bone quality allow for an adequate bone bridge (approximately 5-10mm) and distance from the joint line (approximately 2-4mm), a 3.5mm drill is used to re-create converging bone tunnels. These are connected with curettes and are chamfered similar to a primary Tommy John Surgery.
- If the prior tunnels do not allow for traditional converging bone tunnels, a single-point of fixation is chosen. A pin is placed at the sublime tubercle to allow for at least 4 mm or up to a 5.5 mm reamer to create a unicortical socket to accommodate the size of the graft. There should be adequate bone bridge from the joint line of at least 2 mm and depth of 15mm. The far cortex of the ulna is penetrated with small pin to allow cortical button to pass and flip. Fluoroscopy is used to make sure proximal radioulnar joint is not violated.
Humeral Tunnels
- If the humeral socket and smaller drill tunnels are an appropriate size and in an anatomic location, the humeral socket and small tunnels are re-created similar to as in a primary reconstruction.
- If the humeral tunnel at its inferior location is slightly incorrect, a guide pain is placed at the ideal anatomic location of the humeral tunnel. The pin will most likely pass through the old tunnel by will not be in the center of this tunnel. The guidepin is then over reamed with a 4.5 mm reamer.
- Superior exit tunnels to allow for docking of the graft are then created as in a primary Tommy John Surgery.
- If the humeral tunnel is located at a poor position such as too medial and posterior, a new tunnel can be created completely independent of the previous tunnel. A 4.5mm drill creates a more isometric and anatomic anterior and lateral starting point. In this setting a single, superior exit tunnel is created using a 2mm drill to avoid further compromise to the structural integrity to the epicondyle that could result in fracture. Fixation in this situation will be achieved with a cortical button.
Graft Passing
- The graft is passed through the tunnels as in primary Tommy John Surgery if a traditional ulnar tunnel has been created. If a single-point fixation with cortical button is chosen, the cortical button is passed through the far ulnar cortex and fluoroscopy is used to visualize the cortical button has flipped and is in good position. The graft is tensioned into the ulnar tunnel.
- The graft length is then estimated for humeral tunnel fixation. If standard humeral exit tunnels were created, then the graft is managed as for a primary Tommy John Surgery docking technique.
- If humeral cortical button fixation is required, the graft limb lengths are estimated and sutured with number 1 nonabsorbable suture. The sutures are passed through the single superior epicondyle tunnel. The sutures are then passed through a cortical button and tied over the cortical button with elbow flexion, forearms supination, and a varus stress.
- Elbow motion is ascertained as well as graft isometry.
- The prior graft can be sutured into the new reconstruction with simple 0 non-absorbable sutures.
- The ulnar nerve is transposed subcutaneously if necessary.
- A soft dressing is applied followed by a posterior mold splint that extends past the wrist to ensure complete immobilization. Alternatively, a soft dressing and hinged elbow brace can be applied.
- Post-operative radiographs are obtained at the first office visit.
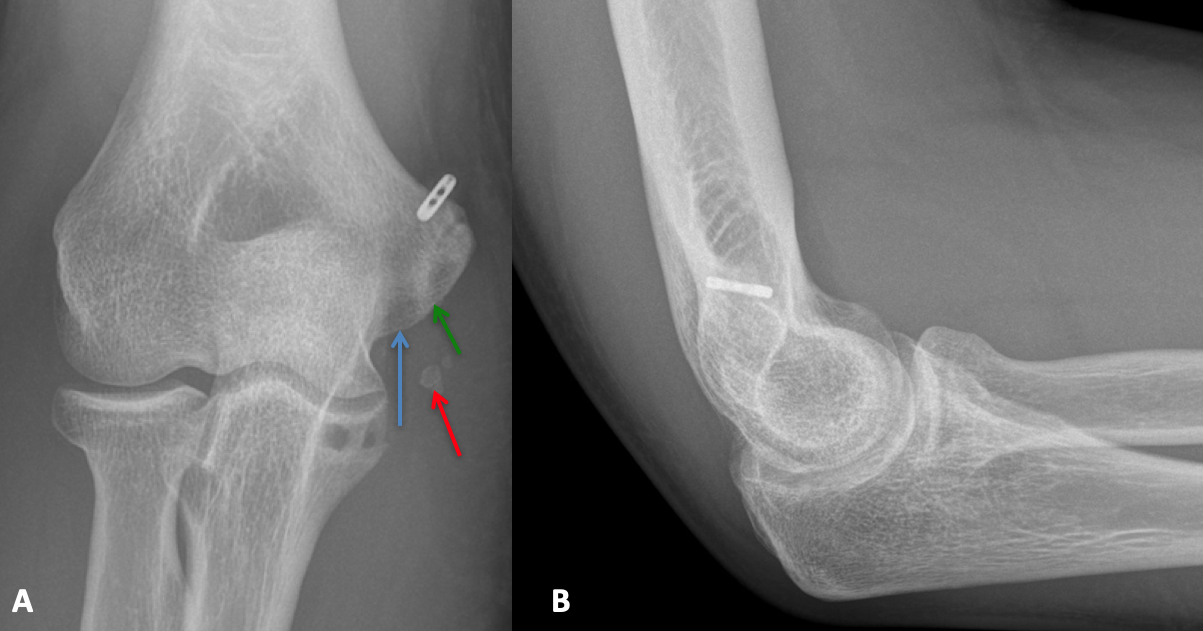
Anteroposterior (A) and lateral (B) X-rays depicting cortical button fixation on the medial epicondyle. The new humeral tunnel is shown with the blue arrow. The prior humeral tunnel is seen with the green arrow. Notice the new tunnel is significantly longer than the original tunnel. The preoperative calcification within the ligament is still seen (red arrow), as the removal of this calcification would have necessitated.
Post-Surgical Rehabilitation
- Rehabilitation following revision Tommy John Surgery is similar to that following primary Tommy John Surgery, although the phases are typically extended by 4-6 weeks depending on how the athlete is progressing. Timing of RTS following revision Tommy John Surgery is typically longer than following primary Tommy John Surgery, and can often be as long as 12-20 months, with some patients taking even longer to reach their preoperative level of competition. Recent studies have found the average time from revision Tommy John Surgery to RTS in major league baseball (MLB) pitchers to be 20.76 months. To an even bigger extent than following primary Tommy John Surgery, special attention must be paid to teaching the pitcher proper pitching mechanics to prevent excess stress on the graft. Similarly, ensuring the pitcher regains strength of both the upper extremity and core is paramount, as is avoiding pitching while the pitcher is fatigued. A slower throwing progression program is also advocated.
Success of Second Time Surgery not as Good
- Unfortunately, the results following revision Tommy John Surgery are inferior to those following primary Tommy John Surgery and is considered between 33%-78%.